Our guest speaker, Jill Fitzgerald, Speech Language Pathologist, discussed the importance of maintaining strong voicing and swallow function in people with Parkinson’s disease.
Swallowing is a life-sustaining motor behavior that transports liquids and nutrients from the mouth to the throat to the esophagus to the stomach. Swallowing is also essential for airway protection. Dysphagia, or difficulty swallowing, will eventually affect most people with Parkinson’s, but the severity is unpredictable. Throat tremors also affect swallowing. Speech therapists help people keep swallowing function.
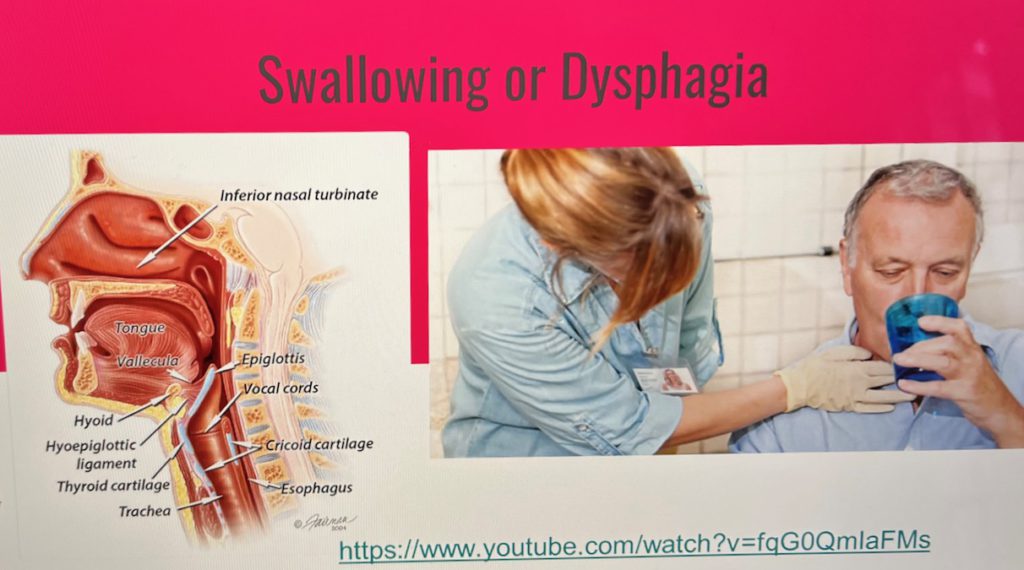
There are three phases of swallowing: Oral, Pharyngeal, and Esophageal
The first or oral phase involves the tongue, the base of which lies deep in the throat. Parkinson’s messes with involuntary control or smooth muscles. The middle or pharyngeal phase involves the epiglottis, which moves up and forward when you swallow. The movement happens in a matter of seconds. The third or esophageal phase squeezes food and liquid down the esophagus, which is made up of smooth and striated muscle, through peristalsis. Speech therapists can’t treat the esophagus. Issues and problems need to be evaluated by a GI doctor.
There are over fifty muscles involved in swallow function which must work together to protect the airway. Speech therapists can provide tricks and techniques to exercise and strengthen them. One that Jill suggests is to pretend to swallow a golf ball, an exercise that strengthens the vocal cords and epiglottis. She also recommends taking a sip of water after every bite you swallow when eating. It’s great for the esophagus and great for the GI system. She also recommends swallowing medication one pill at a time.
Muscle control for the esophagus is sphincteral. We have 50-60 sphincters in our body. The esophagus sphincter muscle is tight at rest and relaxes to open to allow liquid and food to pass through. People who have a significant history of acid reflux need to be aware that it eats away at the esophageal sphincter.
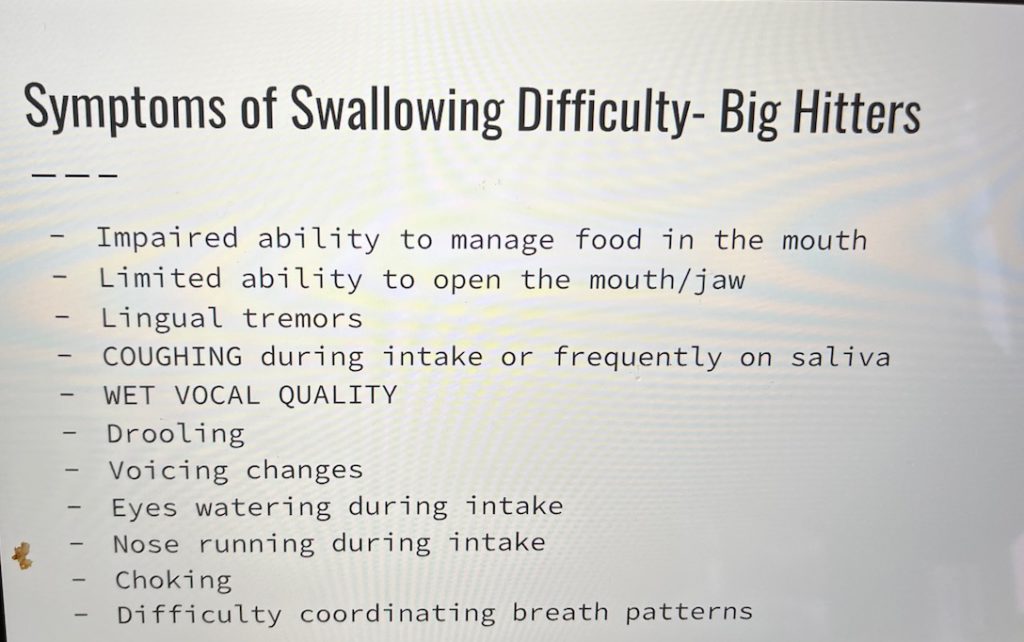
Penetration and Aspiration: Parkinson’s affects the cough reflex that works to keep liquid out of the lungs. When you swallow food or liquid, if a drop or more “tickles” and lands above the vocal cords, it is called penetration. When a drop or more of liquid travels below the vocal cords (or vocal folds) and collects there, it is called aspiration, which can lead to aspiration pneumonia. Symptoms of aspiration pneumonia include changes in mucous production and low grade fever. Speech therapists can do swallow studies as a part of their evaluation to figure out what’s difficult for you and how best to help.
Things to be aware of and look out for:
People with Parkinson’s are at greater risk for malnutrition due to swallowing difficulties, and medication and slow stomach emptying that can leave us feeling full. Jill always recommends a visit with a registered dietician and suggests the website www.eatright.org to locate one near you. Swallowing difficulties can also result in dehydration, which can cause confusion and increases the risk of falls. Jill addressed our questions on how best to hydrate, which can be found here.
If your voice sounds rough or coarse, or your spouse has trouble hearing you (get their hearing checked out first!), Jill suggests asking your doctor for a referral to speech therapy. We associate Parkinson’s with motor issues, but there’s an internal sensory disruption too. Our voices get softer, but we don’t perceive them as so. Dehydration can cause the vocal cords to shrivel up and vocal mechanics to not work as well, resulting in a gravely voice. Lingual and vocal cord tremors affect speech articulation.

Dysarthria, a problem with speech articulation that affects your pronunciation of words, can result from stiffness in the lips. These muscles can be strengthened and strategies speech therapists can help with to significantly improve function. One exercise Jill recommends is to alternate puckering your lips, like you’re giving a big smooch, with smiling wide like a Cheshire Cat. Repeat often.
Voice therapy targets volume, rate of speech, breath control, articulation, breath support, and speaking with intent. Jill is certified for LSVT Loud, an intensive voice treatment program that focuses on loudness, maximum effort, high intensity, and vocal awareness. The perception of your own loudness improves over the four-sessions-a-week four-week program. Another program Jill likes is Speak Out, which includes cognitive exercises, in addition to ones for speech and voice, and requires less sessions per week.
Speech therapists also work with people with cognitive difficulties. Changes in cognitive processes can occur anytime over the course of Parkinson’s. Cognition is not just memory. It includes paying attention, solving problems, remembering to do something, visualizing doing something while getting up to do it.
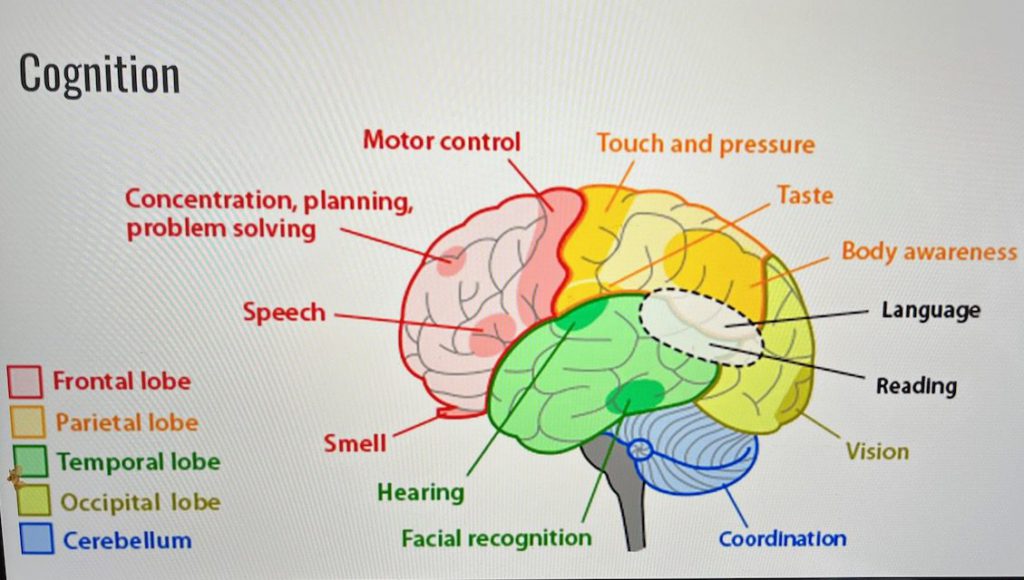
Mild Cognitive Impairment is a new diagnostic term for a difficulty in some area of the brain. Factors such as age, hormones, thyroid disfunction, UTI’s, dehydration, illness, hearing and vision loss, and depression and anxiety can all affect how we function cognitively. Speech therapy can help with mild cognitive impairment. Neuro-psychological testing are done by a psychologist, can take 4-5 hours, and are not always covered by insurance. As a speech therapist, Jill can evaluate under cognitive linguistics, which requires far less time than the testing, to determine working memory and the best course of treatment.
Any more questions? Jill invites you to email her at Jill.Fitzgerald@inova.org or call to schedule to see her at 703-391-3642. She also offers these resources: Radio Parkies and Parkinson’s Voice Project.